Neither too much nor too little
Mr. D comes on all the days I go to the rural clinic in Chengalpet to see me. Not only does he see me, he also goes all the way from his village to the Chengalpet Government Medical College Hospital, which is about 50 Km distance, and sees doctors there. He was there to see me today. Mr. L last saw me 6 years ago. He came in today to see me too, but had never seen a doctor in the past 6 years. Their visits were about 3 hours apart in today's clinic. But when I finished clinic and started to leave, I couldn't help but notice the contrast in the stories of these two men.
Mr. D first came to me 12 years ago with low back pain. After an evaluation, we diagnosed him to have lumbar disc disease with narrowing of the spinal canal. He would go on and off on physiotherapy. Subsequently Mr. D developed high blood pressure and was started on treatment. Then he developed a weakening of the electrical system of his heart called Sick Sinus Syndrome. He was advised to get a pacemaker implantation. He refused due to fear of having some electrical object inserted into his body. No amount of explanation or rationalisation would convince him. So we are managing with medicines to pace his heart. Subsequently he developed prostate enlargement and urinary obstruction. He underwent surgery and sustained complications of the surgery. The past 12 years of our association has been quite dramatic.
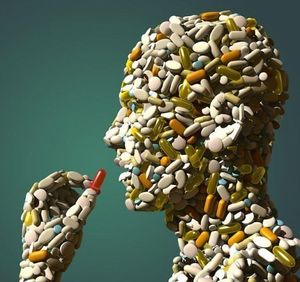
Over the past couple of years Mr. D comes to visit me on almost all days that I go to the clinic. He would often be there before I arrive and would take a token to see me as the first patient of the day. The duration of our encounters gradually increased over time and nowadays he insists on spending anywhere close to 15-20 mins with me in the chamber. Anyone who runs a busy rural out-patient clinic can imagine how tough it can be to spend so much time with one patient while several others are waiting just outside the door looking for an opportunity to barge in. Another new pattern that has started in recent days is that he would go to Chengalpet Government Medical College Hospital early in the morning, see the doctors there, get a prescription and all tablets and on his way home drop by to my clinic and show me everything and ask me for a second opinion on those tablets. Of course it is his right to have such multiple medical opinions. I don't find fault with him for this. I explain the medicines and sort them out for him every time. But what this pattern of behaviour has caused is a dangerous trend of a large number of tablets and medicines in his bag. For example, one time his urologist in the government hospital had prescribed a drug called Tamsulosin which lowers the blood pressure in addition to relaxing the urinary passage. The cardiac specialist had prescribed Amlodipine, a drug that lowers the blood pressure. When he took both of them, he developed severe dizziness and low blood pressure and even fell down one evening. That is when I noticed that he was on both these medicines and had to un-prescribe the Amlodipine. Today he went to Chengalpet Government Hospital and dropped in on his way home. He had a big bag of medicines. One for the burning sensation in his feet, one for dry skin and itching, one for the urinary problem and one for sleep disturbance. He got each of these from a different specialist clinic in the government hospital. It would be a major achievement even for a person who can read the drug labels to sort these tablets and manage them correctly, and Mr. D cannot read or write English.
Mr L came to see me 6 years go. At that time we diagnosed him to have high blood pressure and started him on medications. He is a business man and had a hectic life style back then. He came back today to see me and his case record showed that he had not come to see us over the past 6 years. He had gone completely off the radar. He had not been on any medications for the high blood pressure. Today when I recorded his blood pressure it was extremely high at 240/140 mmHg. Not only that, his blood tests revealed that he had started developing early kidney disease. When I asked him what made him go off medications and why he never sought any medical help over the past years, he replied that he was feeling alright and so did not feel the need to go to a doctor.
Stories like those of Mr. D and Mr. L are not uncommon. The biggest challenge I face on a daily basis is to convince a person who feels absolutely normal and well that they must take tablets for their diabetes and high blood pressure, which are silently doing damage in their body. This is the challenge with Mr. L who did not see a reason to take tablets when he was doing fine. Mr. D's case is the polar opposite where multiple vague bodily complaints push him to repeatedly seek medical care. The specialised medical care system sees him as a collection of body parts and treat the individual diseased parts. My teacher used to tell me that it takes, 3 C's - competence, confidence and conviction to tell a patient that they do not need medicines and they are fine. I subsequently realised that along with the 3 C's it takes time and effort to sit with a patient, assess them, understand them clearly and make a decision that they are normal. The busy government doctor in the general hospital out patient clinic does not have the luxury of time. So they are often unable to tell a patient that they are normal and they don't need medicines. They end up prescribing medicines and when a patient navigates the fractured super specialised health system, the result is a potpourri of medications.
On one hand I have to tell the likes of Mr. L that they cannot wait for symptoms and problems to occur, and they have to take care of their health even if they are feeling perfectly normal. And on the other hand I have to tell people like Mr. D that sometimes the best thing to do would be to manage minor problems at home without going to a doctor. Going to many doctors will only confuse the situation. The hope is that Mr. D and Mr. L do not meet and discuss what I told them. There is probably the ideal middle path between these two extremes and I am trying to figure out how to tell my patients to tread that path.
Comments
Post a Comment